The world inside a mother’s womb is a fascinating place where a new life unfolds. One of the critical aspects of this newfound life is its genetic structure, the chromosomes, which carry the unique blueprint of the individual. Chromosomal abnormalities are alterations in this blueprint, which can lead to conditions like Down Syndrome, Patau Syndrome, and Edwards Syndrome, with varying impacts on the individual’s health and development. As maternal age increases, so does the risk of these abnormalities. Thus, it becomes imperative to understand the importance of prenatal testing. These tests aim to detect any chromosomal abnormalities early, allowing for informed decisions on further management and preparedness for potential implications.
What are Chromosomal Abnormalities
Understanding Chromosomal Abnormalities
Chromosomal abnormalities are variations or disorders that occur when there is a discrepancy in the number or structure of chromosomes in a cell. These irregularities can occur due to several factors, including genetic mutations, errors during cell division, exposure to radiation, or toxins. They can result in a wide array of health problems, developmental issues, and in some cases, can be fatal.
Common Types of Chromosomal Abnormalities
Three common chromosomal abnormalities are Down Syndrome, Patau Syndrome, and Edwards Syndrome. Down Syndrome, also known as trisomy 21, is caused by an extra chromosome 21, either in part or in whole. It is the most common chromosomal abnormality, affecting cognitive abilities, physical growth, and causing characteristic facial features.
Patau Syndrome, less common but more severe, is also known as trisomy 13. Infants with Patau syndrome usually have severe intellectual disability, along with physical abnormalities in many parts of the body. This disorder can potentially lead to heart defects, brain or spinal cord abnormalities, very small or poorly developed eyes, or extra fingers or toes.
Edwards Syndrome, trisomy 18, is caused by an additional chromosome 18. It impacts multiple organ systems and is characterized by growth deficiency, heart malformations and numerous other abnormalities. It is associated with a high mortality rate: many fetuses with this condition do not survive full term, and infants that do survive often don’t live past their first year.
Impacts of Chromosomal Abnormalities on Health and Development
Every individual inherited 23 chromosomes from their mother and 23 from their father, forming 23 pairs. These chromosomes contain genes that provide specific instructions for bodily processes — from growth, development, and function. Deviations or variations in this genetic structure can disrupt these processes, leading to multiple health problems and developmental issues.
Prenatal Testing for Chromosomal Abnormalities
Prenatal testing for chromosomal abnormalities can help detect these conditions in a fetus before birth. Techniques include maternal serum screening tests, cell-free DNA testing, amniocentesis, and chorionic villus sampling (CVS). These tests can provide essential information about the chromosomal health of a developing fetus, helping healthcare providers and families prepare for a baby with special needs or make difficult decisions about the pregnancy.
While these prenatal tests have associated risks, including false positives, false negatives, and potential harm to the fetus or mother, they have proven instrumental in early detection and management of chromosomal abnormalities.
Prenatal testing is a decision that warrants careful consideration.
Any individuals or couples thinking about undergoing these tests should engage in thorough discussions with their healthcare provider. This is to understand the potential pros, cons, and risks involved, helping them to make a well-informed decision.
The Importance of Prenatal Testing
Understanding the Importance of Chromosomal Abnormalities Prenatal Testing
The significance of prenatal testing for chromosomal abnormalities cannot be overstated as it aids in the early detection of potential health concerns during pregnancy. Such tests are instrumental in identifying genetic disorders like Down syndrome, Edwards Syndrome, Patau Syndrome, and a range of other conditions that could affect a baby’s health and overall development.
Risks Associated with Chromosomal Abnormalities
Chromosomal abnormalities carry inherent risks. Some of these conditions can lead to severe intellectual disability, developmental delay, physiological malformations, and problems with the heart, skeletal system, or other organs. Early detection through prenatal testing can dramatically improve an infant’s prognosis and overall quality of life.
One of the most common chromosomal abnormality conditions, Down Syndrome, occurs due to the presence of an extra copy of chromosome 21. Edwards syndrome and Patau’s syndrome, while less common, result from extra copies of chromosomes 18 and 13, respectively, and are often associated with severe physical and intellectual challenges.
Maternal Age and Chromosomal Abnormalities
Maternal age plays a significant role in the risk of conceiving a child with chromosomal abnormalities. The risk gradually increases with maternal age, particularly for women who are 35 years old or older. For example, the risk of a woman aged 25 having a baby with chromosomal abnormalities is about 1 in 1,200. At age 35, the risk increases to approximately 1 in 350, and by age 45, it advances to around 1 in 30.
Early Detection and Preparation via Prenatal Testing
Prenatal testing for chromosomal abnormalities can offer expectant parents vital information about their baby’s health before birth. There are several types of prenatal tests, including screening tests and diagnostic tests.
Screening tests estimate the risk of the fetus having certain chromosomal disorders, while diagnostic tests can detect if the fetus actually has a certain disorder. These tests not only enable healthcare providers to make informed decisions about treatment and management options but also equip parents to prepare emotionally, financially, and practically for health issues their child may face.
Emotional and Financial Implications
Having a child with chromosomal abnormalities can bring on an array of emotional and financial implications. Emotionally, a diagnosis can trigger a grieving process as parents navigate feelings of shock, denial, guilt, sadness, and acceptance.
Financially, costs can skyrocket due to medical treatment, surgeries, therapy, special education requirements, and long-term care. Early detection through prenatal testing can give parents the opportunity to anticipate these costs and seek resources and support systems, thus reducing future stress and anxiety.
Assessing prenatal chromosomal abnormalities is key, not only because it offers vital medical data, but it also equips families and medical professionals to adequately prepare for the arrival of a child with special needs.

Techniques in Prenatal Testing for Chromosomal Abnormalities
Exploring Non-Invasive Prenatal Testing for Chromosomal Abnormalities
Non-Invasive Prenatal Testing (NIPT) provides a safer way to ascertain chromosomal abnormalities without any invasive procedures. Conducted typically between the 10th and 14th week of pregnancy, this method utilizes fetal DNA present in the mother’s bloodstream. With a single blood sample from the expecting mother, it’s possible to detect potential chromosomal irregularities encompassing Down Syndrome, Edwards Syndrome, and Patau Syndrome, among others.
NIPT’s notable precision and minimal risks to both the fetus and the mother have made it a favorable choice. It boasts a detection accuracy exceeding 99% in identifying Down Syndrome, and around 97–98% for Edwards and Patau Syndromes. While not absolute, a positive outcome from an NIPT signifies a heightened risk of a chromosomal irregularity.
Ultrasound Techniques
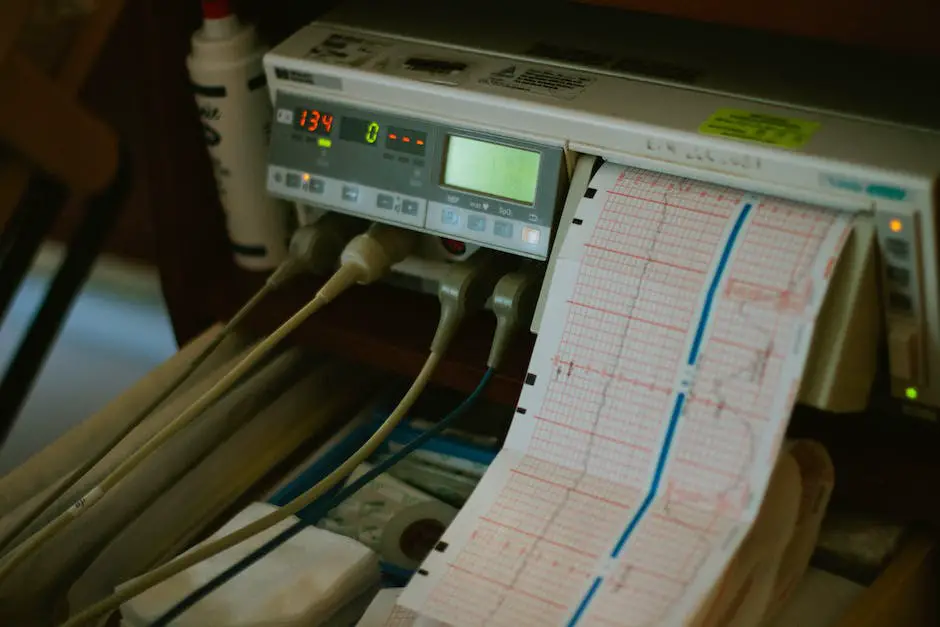
Ultrasound is another non-invasive technique used for prenatal testing. It uses sound waves to create images of the baby in the womb. While it’s usually conducted multiple times throughout the pregnancy, the second-trimester ultrasound, or “anatomy scan,” is particularly crucial for detecting chromosomal abnormalities. This is generally done between 18 and 22 weeks of gestation.
Some chromosomal abnormalities may cause physical abnormalities that can be detected through ultrasound. However, not all conditions result in detectable physical symptoms, so ultrasound does not guarantee complete certainty.
Amniocentesis
This invasive prenatal test involves taking a small sample of the amniotic fluid surrounding the fetus during pregnancy, typically performed between the 15th and 20th weeks of gestation. The collected fluid contains fetal cells, which can then be analyzed for chromosomal abnormalities.
While Amniocentesis provides a high degree of accuracy, it carries a minimal risk of miscarriage. Therefore, it’s typically reserved for women who present an increased risk of chromosomal abnormalities, as determined by earlier screenings.
Chorionic Villus Sampling (CVS)
Another invasive prenatal testing method is Chorionic Villus Sampling. It involves collecting a small sample of cells from the placenta, usually between the 10th and 13th weeks of pregnancy. These cells can then be tested for chromosomal abnormalities.
CVS tends to be performed early in the pregnancy than amniocentesis and gives comparably accurate results. However, it carries a slightly higher risk and so is typically recommended for women at increased risk of certain genetic conditions.
It’s important to keep in mind that while these tests can offer a high degree of dependability, none of them can deliver a 100% certainty. Aspects such as the timing of the test, the age of the mother, and the specific chromosomal abnormality being studied can all affect the precision and interpretation of the results. In considering prenatal testing for chromosomal abnormalities, it’s always crucial to fully discuss these factors, as well as the possible risks and advantages, with healthcare professionals.

Understanding the Results of Prenatal Testing
Interpreting Prenatal Test Outcomes
Prenatal testing is a medical process carried out during pregnancy to scrutinize the progress and health of the baby in utero. These examinations often involve checking for potential chromosomal irregularities such as Down syndrome, trisomy 18, trisomy 13, along with conditions linked to superfluous or lacking chromosomes.
Interpreting Negative and Positive Results
Test results may be labeled as ‘negative’ or ‘positive.’ A ‘negative’ result signifies that the tests did not detect any chromosomal abnormalities and the child is likely to be born without any chromosomal disorders. However, while a negative result lowers the potential risk, it does not guarantee the absence of chromosomal abnormalities.
A ‘positive’ result, on the other hand, means the test has detected potential chromosomal abnormalities. But this doesn’t automatically mean the baby will be born with a disorder. Often, a positive result points out an increased risk and the need for further testing.
Understanding the Accuracy of Prenatal Testing
The accuracy of these prenatal tests is measured in terms of sensitivity and specificity. Sensitivity refers to the test’s ability to correctly identify pregnancies with chromosomal abnormalities, while specificity pertains to its ability to accurately identify pregnancies without these abnormalities. However, no test is 100 percent accurate, and there might be false-positive or false-negative results. Therefore, a positive result does not always signal an issue, just as a negative result does not always indicate the absence of one.
Next Steps After a Positive Result
A positive result is often followed by additional confirmatory testing. These could include diagnostic tests like amniocentesis or chorionic villus sampling (CVS), which provide a more accurate analysis of the baby’s chromosomes. However, these tests carry a small risk of miscarriage, and thus the risks and benefits should be thoroughly discussed.
Genetic counseling is another important step following a positive prenatal testing result. Genetic counselors offer information, guidance, and support. They explain what the test results mean, provide more context about the specific chromosomal abnormality detected, suggest further tests, and discuss the potential implications for the child and the entire family.
Pregnancy Management Options
Based on the results of confirmatory tests and counseling, parents can then explore choices for managing the pregnancy. Options might include preparing for a child with special needs, considering adoption, or making a decision about continuing or terminating the pregnancy. However, these are highly personal decisions that depend on a variety of factors including medical, ethical, cultural, religious, and personal beliefs. The goal of prenatal testing is to provide parents with necessary and timely information so they can make informed decisions about their pregnancy.
As we navigate the journey of prenatal testing, understanding its purpose, techniques, and results become crucial. Each method, whether non-invasive like ultrasound and blood tests, or invasive like Amniocentesis and Chorionic Villus Sampling, serves an irreplaceable role in early detection and risk assessment. Interpreting the results can, at times, be complex, with intertwined factors like false positives and individual risk profiles, necessitating meticulous deliberation. Regardless of the outcome, the information gathered is invaluable, granting prospective parents the power to make informed decisions. Therefore, prenatal testing for chromosomal abnormalities serves as an indispensable asset in the noble pursuit of nurturing the gift of life.
FAQ
What are the 4 prenatal tests?
Prenatal tests come in a variety of forms, but four are frequently suggested:
- Ultrasound: This popular prenatal test creates images of the developing fetus using sound waves. It is used to determine the approximate date of delivery, determine the presence of multiple pregnancies (twins, triplets, etc.), evaluate the growth and development of the fetus, and screen for specific birth defects or anomalies.
- Screening for Maternal Serum Alpha-Fetaprotein (MSAFP): A blood test known as MSAFP is done between weeks 15 and 20 of pregnancy. It gauges the mother’s blood’s alpha-fetoprotein concentrations. A higher risk of certain birth defects, like spina bifida or Down syndrome due to chromosomal abnormalities, may be indicated by abnormal levels.
- Chorionic Villus Sampling (CVS): CVS is an invasive prenatal test performed between the 10th and 13th weeks of pregnancy. For genetic testing, a tiny sample of placental tissue (chorionic villi) must be removed. Chromosome abnormalities and genetic disorders can be detected by CVS, although compared to other tests, there is a slight risk of complications.
- Amniocentesis: This intrusive prenatal test is usually carried out in the fifteenth and twentieth weeks of pregnancy. In order to obtain a sample of amniotic fluid, a needle is put through the mother’s abdomen and into the amniotic sac during this procedure. Next, chromosomal abnormalities and genetic disorders are examined in this fluid. Amniocentesis has a small chance of complications, just like CVS.
What does prenatal testing test for?
The following are some of the particular conditions and goals that prenatal testing can identify or screen for:
- Abnormalities related to genes and chromosomes: Prenatal testing can detect the presence of an extra copy of chromosome 21 in cases of Down syndrome (trisomy 21). Testing for the presence of extra chromosomes—specifically, chromosomes 18 and 13, respectively—can also reveal the existence of Edwards Syndrome (trisomy 18) and Patau Syndrome (trisomy 13). Other Chromosome Abnormalities: In addition to the common trisomies, certain tests, such as amniocentesis and chorionic villus sampling (CVS), can identify a broad variety of other chromosomal abnormalities.
- Neural Tube Defects: Maternal serum alpha-fetoprotein (MSAFP) screening may reveal a heightened risk of neural tube defects in the developing foetus, which can lead to spina bifida and anencephaly.
- Sex Chromosome Abnormalities: Tests can identify sex chromosome-related disorders such as Klinefelter syndrome (XXY) and Turner syndrome (monosomy X).
- Genetic Disorders Inherited: Prenatal testing can detect certain genetic disorders, like sickle cell disease or cystic fibrosis, that are inherited.
- Fetal Well-Being and Development: Ultrasound exams are used to evaluate the health of the fetus, placenta, and amniotic fluid in addition to tracking fetal growth and looking for physical anomalies.
- Multiple Pregnancies: An ultrasound can reveal whether a mother is carrying twins, triplets, or more fetuses.
- Maternal Health and Complications: In addition to screening for infections like rubella, routine prenatal screenings also evaluate the mother’s health, including blood pressure, blood sugar levels (for gestational diabetes), and other conditions.
Is prenatal testing required?
Here are some important things to think about:
- Routine Prenatal Care: It is recommended that expectant mothers receive routine prenatal care, which entails check-ups on a regular basis, consultations with a healthcare professional, and a variety of screenings and tests. Regular screenings aid in keeping an eye on the mother’s and the fetus’s development and health.
- Informed Decision-Making: Prenatal testing is typically provided as an option, and people are urged to choose their tests wisely. The choice to have prenatal testing done should be based on the patient’s unique situation, preferences, and conversations with medical professionals.
- High-Risk Pregnancies: To evaluate and manage risks in situations where there are recognized risk factors or signs of possible complications, medical professionals may suggest particular prenatal testing. For instance, people who are advanced in age (usually 35 or older), have a family history of genetic disorders, or have experienced difficulties during a previous pregnancy might be recommended for further testing.
- Ethical and Legal Considerations: In some regions, there may be legal or ethical considerations related to prenatal testing. For example, certain regions might mandate that medical professionals offer specific tests or counsel patients regarding options for prenatal testing.
- Patient Autonomy: Pregnant people have the right to make healthcare decisions for themselves, and the decision to have prenatal testing done is ultimately a personal one. When it comes to giving people the knowledge, direction, and encouragement they need to make wise decisions, healthcare providers are essential.
What is the difference between prenatal testing and genetic testing?
Genetic testing is a more general term that includes a range of tests intended to determine an individual’s genetic composition and to identify genetic conditions or predispositions, whereas prenatal testing concentrates on tracking and evaluating the health of the mother and the fetus during pregnancy. Genetic testing is not exclusive to prenatal care; it can be done at any point in an individual’s life. Prenatal testing may involve genetic testing when the objective is to evaluate the genetic health of the fetus.
What prenatal testing is recommended?
Here are some common prenatal tests that are often recommended or offered as part of routine prenatal care:
- Ultrasound Examinations
- Non-Invasive Prenatal Testing (NIPT)
- Carrier Screening
- Glucose Screening
- Group B Streptococcus (GBS) Screening
- Amniocentesis and Chorionic Villus Sampling (CVS)
- Fetal Non-Stress Test (NST) and Biophysical Profile
It is imperative to bear in mind that the choice to have particular prenatal tests should be taken after consulting with a healthcare professional who can customize recommendations to your particular situation and offer advice based on your health and the status of your pregnancy. Furthermore, the accessibility of specific tests might change based on your location and the policies of your healthcare provider.