The application of genetic testing in medicine has far-reaching implications, with one of the most prevalent being its role in early cancer detection. This article aims to apprise the reader about the intricate workings of genetic tests in identifying colon cancer and address the complexities surrounding this highly scientific procedure. As we navigate through the complexities of colon cancer, the distinguishing features of genetic tests, their interpretations, and their social/legal implications, we aim to enlighten our readers about how modern medicine uses genetic markers to protect against this grave, yet often preventable, disease.
Understanding Colon Cancer
Colon Cancer: A Brief Overview
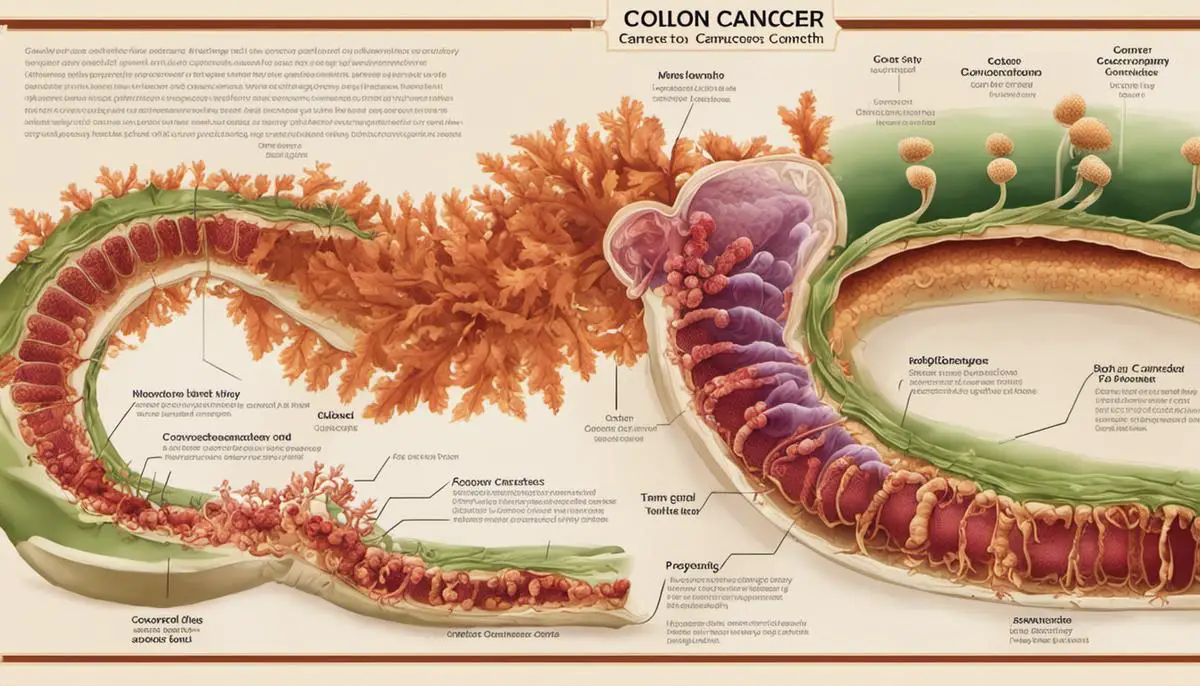
Colon cancer, also referred to as colorectal cancer, begins in either the colon or rectum. It typically starts as small noncancerous (benign) clumps of cells known as polyps that form on the inside of the colon. Over time, these polyps can become cancerous, with some types presenting a higher risk than others.
Genetics and Colon Cancer
Mutations in certain genes may increase the chances of developing colon cancer. Germline mutations are inherited from a parent and are present throughout a person’s life in virtually every cell in the body. They are responsible for about 5% to 10% of colon cancers. Acquired (or somatic) mutations occur at some point during a person’s life and are only present in cells that become cancerous.
Two common mutations associated with increased colon cancer risk include Lynch syndrome (hereditary non-polyposis colorectal cancer or HNPCC) and Familial Adenomatous Polyposis (FAP). Other inherited genes linked to increased colon cancer susceptibility include MUTYH-associated polyposis (MAP) and Peutz-Jeghers syndrome.
Symptoms of Colon Cancer
Not all individuals will experience symptoms of colon cancer in the early stages. As the condition progresses, symptoms may include changes in bowel habits (diarrhea, constipation, or narrowing of the stool for more than a few days), bleeding from the rectum or blood in stool, persistent cramping or pain in the abdomen, fatigue, weakness or unexplained weight loss.
Prevention and Early Detection: Role of Genetic Tests
While colon cancer cannot always be prevented, regular screening tests such as colonoscopies can greatly increase the chance of detecting this type of cancer in its early stages when treatment is most likely to be successful. Recognizing and understanding genetic risks can also help in early detection and prevention.
Genetic tests can help to identify individuals who are at higher risk due to inherited gene mutations. By identifying these gene mutations, healthcare providers can recommend more frequent or intensive screening procedures or preventive treatments even before symptoms develop. It’s crucial to know that genetic testing generally doesn’t tell whether a person will develop colon cancer, but can only tell whether a person carries certain genes that are associated with an increased risk.
The Importance of Genetic Testing
There are numerous benefits of genetic testing, particularly for those with a family history of colon cancer, since it can pinpoint even asymptomatic carriers who may pass the mutation onto their children. Even if a person doesn’t have a gene mutation, the test can still provide a sense of relief from uncertainty and help people make informed decisions about managing their health care.
However, interpreting the result of a genetic test can be complex, and it’s recommended to have the aid of a genetic counselor or other trained medical professionals to understand what the results could mean for your health.
Understanding the Role of Lifestyle & Genetics in Colon Cancer
Reducing the risk of colon cancer involves a comprehensive approach that combines both lifestyle modifications and medical strategies. Adopting a healthy diet, increasing physical activity, moderating alcohol intake, and quitting smoking all contribute to colon cancer prevention. Additionally, genetic testing is becoming an increasingly valuable tool for early detection and intervention.
The Role of Genetic Testing in Cancer Detection
The Role of Genetic Testing in Detecting Colon Cancer
As part of this comprehensive strategy, genetic testing offers the capability to identify alterations in chromosomes, genes, or proteins, which can suggest inherited gene mutations linked to cancers such as colon cancer. Individuals who have a known family history of colon cancer, or those who exhibit concerning symptoms, may particularly benefit from such tests, helping them seek early and appropriate treatments.
Purpose of Genetic Testing in Cancer Detection
The primary goal of genetic testing in cancer detection is to identify the presence of genetic mutations that are known to contribute to the risk of developing cancer. In the case of colon cancer, these include inherited syndromes such as hereditary nonpolyposis colorectal cancer (HNPCC) or Lynch syndrome, and familial adenomatous polyposis (FAP).
Genetic testing, when used as a proactive measure, allows individuals to make informed decisions about their health, and can often lead to earlier and more accurate cancer detection. Furthermore, results from genetic tests can provide valuable information for the entire family, highlighting potential genetic risks and encouraging family members to take more proactive steps towards their health.
Procedure for Genetic Testing
The process for genetic testing often begins with a blood or saliva sample, which is then sent to a lab for analysis. In the lab, technicians will examine the sample for specific changes in chromosomes, DNA, or proteins, depending on the type of test. The entire process takes about several weeks.
To facilitate the understanding and interpretation of the test results, it is usually recommended that an individual undergo genetic counseling both before and after the test. This helps individuals have a clear understanding of the risks and benefits of testing and helps them make an informed decision.
Benefits and Limitations of Genetic Testing for Colon Cancer
There are several potential benefits to genetic testing for colon cancer. Perhaps the most significant is the potential for early detection and intervention. If a specific mutation is identified, more frequent and comprehensive screenings may be conducted, potentially catching any cancerous cells at an earlier stage.
However, it is important to be aware of the limitations and potential drawbacks of genetic testing. Positive results do not necessarily mean that an individual will definitely develop colon cancer, and negative results do not rule out the possibility. Some genetic tests can miss certain mutations, and not all inherited mutations that can lead to colon cancer are currently known.
Additionally, genetic testing can lead to significant emotional stress and anxiety about potential health outcomes. It can also lead to increased costs due to more frequent screening and prevention strategies. Furthermore, there may be potential implications for insurance coverage based upon the results.
In the modern age of medical innovation, genetic testing serves as an invaluable tool, providing crucial insight into possible cancer risks. These tests, however, should be undertaken judiciously, under the expert supervision of healthcare professionals who can offer a comprehensive interpretation of results and strategic advice for future steps. Prior to moving forward with the testing process, it is of massive importance to consider the emotional and financial implications that the procedure may entail.
Specific Genetic Tests for Colon Cancer
Understanding Colon Cancer and the Role of Genetic Testing
Colon cancer is a type of malignancy that originates in the colon or the rectum, both parts of our body’s digestive system. If left unchecked, certain mutations in the cells of the colon could multiply erratically, forming a tumor that could potentially lead to colon cancer. The advent of genetic testing has made it feasible to pinpoint these harmful mutations before they evolve into severe health hazards. Genetic tests particularly designed for colon cancer detection can include an array of methods such as fecal blood tests, colonoscopies, DNA stool tests, sigmoidoscopies, and others.
Fecal Immunochemical Test (FIT)
The Fecal Immunochemical Test (FIT) is a non-invasive test that can identify small amounts of blood in the stool, which can be an early sign of colon cancer. During a FIT test, patients collect a stool sample at home, which is then analyzed in a laboratory. The test, recommended yearly for individuals over the age of 50, is efficient in detecting most large colorectal cancers. However, FIT may miss smaller cancers or polyps that are not yet bleeding.
Colonoscopy
A colonoscopy is an invasive but highly accurate test that can detect colon cancer or precancerous polyps. During a colonoscopy, a small camera attached to a flexible tube is inserted into the rectum and advanced to the colon. This enables the physicians to visually inspect the entire colon and rectum for abnormalities or polyps. If any are seen, they can be biopsied or removed during the procedure. Specimens are then sent to a lab for testing to determine if they are cancerous, precancerous or benign.
DNA Stool Test
Another type of testing used for colon cancer detection is the DNA stool test, such as Cologuard. Like FIT, these tests involve the patient providing a stool sample that is then analyzed in a lab. However, instead of just checking for blood in the feces, DNA stool tests also look for abnormal DNA which colorectal cancers or precancerous polyps may shed into the stool. While this test does have a higher sensitivity than FIT, it also has a higher chance of false-positive results.
Genetic Counseling and Screening
It’s also essential to consider genetic counseling and screening options for colon cancer. This is particularly impactful for people at high risk of colon cancer due to a strong family history or inherited syndromes like Lynch Syndrome (hereditary nonpolyposis colorectal cancer – HNPCC) or Familial Adenomatous Polyposis (FAP). Specific gene tests can be conducted to identify the mutations in these genes, which will enable doctors to better strategize a surveillance and prevention plan for those individuals.
Factors To Consider
While genetic tests for colon cancer have good accuracy, they are not 100% reliable. Some test results may return false positives, indicating cancer while there isn’t one, or false negatives, missing out on detecting colon cancer. Therefore, it’s crucial for the patient to discuss the outcome with their healthcare provider.
Practical considerations for each genetic test include invasiveness, preparation, cost, and frequency of testing suggested by the healthcare provider. Ensuring valid health insurance can cover some tests; others may need out-of-pocket expenses.
For individuals deemed to be at standard risk, routine tests like colonoscopies are typically advised from the age of 50. However, those with a higher risk because of family history or genetic predispositions might need to begin these check-ups sooner and conduct them more regularly. This is because regular screenings lead to early detection of colon cancer, making it significantly more treatable and increasing the patients’ survival rate considerably.

Interpreting the Results of Genetic Tests
A Deeper Dive into Gene Test Results for Colon Cancer
Genetic testing has become a vital resource in understanding and predicting colon cancer. These test results can appear quite complex, sometimes appearing positive, negative, unclear, or showing variants of uncertain significance. Let’s take a closer look at what these results mean.
A positive result signifies that the person being tested carries a specific genetic mutation linked with a higher risk of developing colon cancer. However, a positive result isn’t a disease prediction. It merely indicates the presence of a gene variant associated with colon cancer; it doesn’t forecast if, when, or how severely the disease may manifest.
If the result is negative, it means that the individual doesn’t carry the tested genetic mutation, reducing their genetic risk of colon cancer. Nevertheless, a negative result doesn’t entirely nullify the risk. Traditional factors such as age, diet, or exposure to environmental toxins can still contribute to the likelihood of developing the disease.
Inconclusive results are more indistinct, indicating that the test could not definitively determine the presence of a genetic mutation connected to colon cancer. Any such unclear results usually indicate further evaluation or regular check-ups are necessary.
A result showing a variant of uncertain significance (VUS) states that although a mutation or change in your DNA was found during the test, the significance and implications of this particular change in relation to colon cancer are unclear.
Scope of Information from Genetic Tests and Next Steps
Genetic tests can provide a range of information, from confirmation of a suspected diagnosis based on symptoms, to a better understanding of the risk or likelihood of developing colon cancer. Immediate relatives of a person who tests positive for a colon cancer-causing gene mutation can also take the test to clarify their own risk.
However, genetic testing is only one component of a comprehensive health evaluation and care. Consulting with healthcare providers is essential after receiving test results. Depending on the results, they may recommend more frequent screenings, changes in diet or lifestyle, or prophylactic (preventive) surgeries as well as specific therapies if the cancer is present.
Understanding the Emotional Impact of Colon Cancer Genetic Test Results
The emotions tied with receiving genetic test results for colon cancer can be wide-ranging. It’s normal to grapple with feelings of anxiety, unease or confusion, especially when faced with positive or unclear results. Conversely, a negative result can evoke a wave of relief and reassured certainty.
No matter what emotions surface, it’s key to connect with support systems during this time. Channels to consider can include a genetic counselor, mental health specialists, community support groups, or confiding in trusted loved ones. These resources can provide guidance in managing emotions, interpreting test results, and planning potential next steps.
Remember, genetic tests are a valuable tool that provides information to guide your future health care choices. However, having a gene mutation doesn’t necessarily mean you’ll develop colon cancer and vice versa. Given the swift advancement in genetic technology and understanding, continuous research and frequent consultations with healthcare providers are necessary to stay up-to-date.
Ethical, Legal, and Social Implications of Genetic Testing for Colon Cancer
Considering the Ethical Questions of Colon Cancer Genetic Testing
Exploring genetic testing for colon cancer raises an assortment of ethical dilemmas. The central concern is about the autonomy and informed consent of individuals. It’s crucial to fully understand the possible repercussions of test results, which can profoundly influence health and lifestyle decisions. This includes the potential for false positives and negatives, each of which carries substantial emotional and psychological burdens.
Additionally, the concept of genetic determinism becomes a significant consideration. Once an individual discovers they have a genetic predisposition to colon cancer, they may adopt a fatalistic view, thinking their fate is predetermined due to their genetics. This mindset could trigger unwarranted anxiety, stress, and behavioral changes based on a mistaken sense of inevitability.
Legal Aspects of Genetic Tests for Colon Cancer
In terms of legality, the Genetic Information Nondiscrimination Act (GINA) of 2008 affords protection to individuals against genetic discrimination in health insurance and employment in the United States. However, the law does not cover life insurance, disability insurance, or long-term care insurance. This raises concerns about potential discrimination based on genetic predisposition to diseases like colon cancer.
Moreover, there are legal questions regarding who owns genetic information, whether or not such information can be patented, and how consent should be approached and obtained. The privacy of genetic information and the potential for its misuse by insurance companies, employers, and other entities remains a significant concern.
Social Implications of Genetic Testing
On the social front, the potential stigma attached to individuals identified with a genetic predisposition to colon cancer cannot be overlooked. This can lead to social discrimination, which can further impact mental and emotional health. Similarly, the dissemination of genetic information within the family can lead to tension, as it might not just reveal risks to the individual tested, but also to their family members.
Furthermore, the economic disparities in access to genetic testing and subsequent care contribute to social inequity. There are also concerns about the fair allocation of resources, given that genetic testing for colon cancer, subsequent surveillance, and preventative procedures are relatively expensive.
The Moral Complexities of Genetic Tests
The ability to gauge one’s predisposition to develop colon cancer via genetic tests introduces moral complexities. The decision made post-testing intersects with moral norms around prevention and treatment. There’s also the quandary about whether to share genetic risk information with family members, raising ethical issues around beneficence, non-maleficence, and justice.
Therefore, while genetic testing for colon cancer indeed offers the potential to reduce mortality and advance personalized medicine, the ethical, legal, and social implications inherent in the process require careful consideration and continuous dialogue.

The science of genetic testing is both a boon and a bane. With potential to predict our predispositions to diseases like colon cancer, it integrates the future of our health into our hands now. Yet it also opens up Pandora’s box of ethical, legal, and social quandaries. Our understanding of these intricacies allows us to harness the benefits while mitigating potential challenges. As science gallops forward, the way we employ genetic testing, interpret its results, and address its repercussions will largely determine its ultimate potential in advancing human health.
