Functional dyspepsia, a condition affecting the upper digestive tract, remains of significant concern due to its prevalence and impact on daily life. Through this comprehensive overview, an audience seeking to understand the nature of this unique disorder can engage with substantial information, including what functional dyspepsia entails, the people it affects, and its prevalence. This study is further extended to provide an in-depth look at its symptoms, causes, and the diagnosis process. Readers will also find the evaluation of treatment options and lifestyle management incredibly enlightening, offering critical insights into these holistic means of addressing the condition.
What is Functional Dyspepsia?
Understanding Functional Dyspepsia
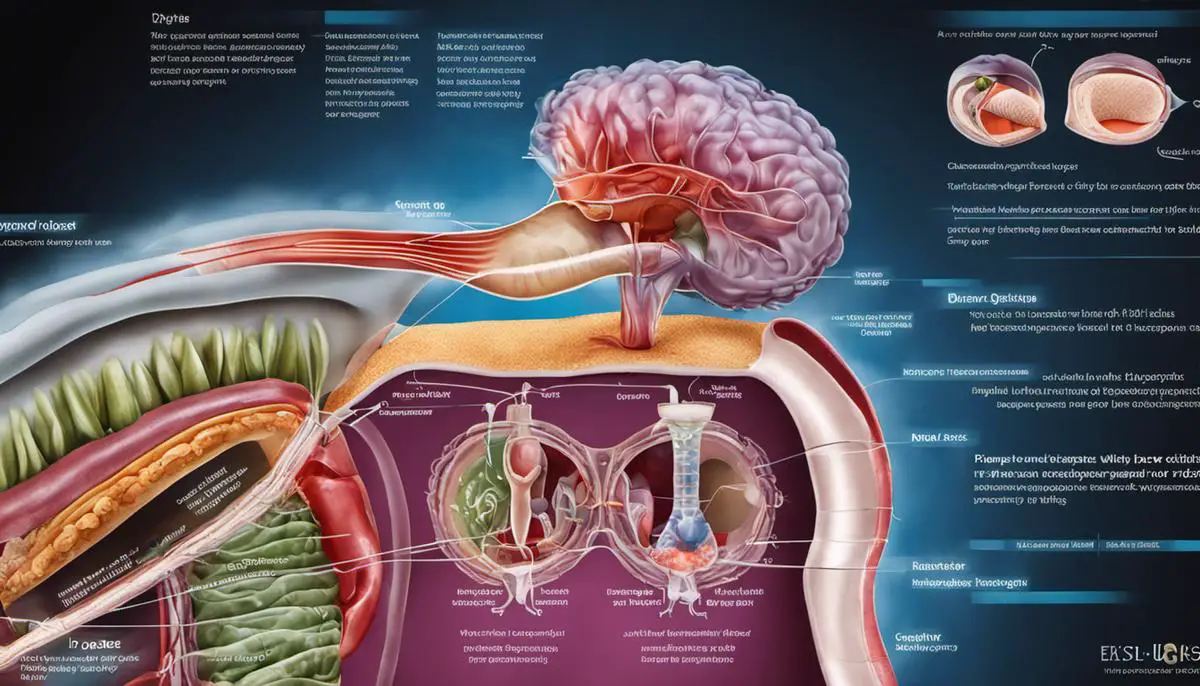
Functional Dyspepsia (FD), commonly known as indigestion, is a medical term used to describe a collection of symptoms that occur in the upper gastrointestinal tract. It affects the stomach and the first part of the small intestine, known as the duodenum. Functional dyspepsia is called “functional” because the organ’s structure or physical appearance does not explain the symptoms a patient experiences. There are no visible signs of damage or disease upon investigation, like an endoscopic examination, but the stomach functions poorly.
Types of Functional Dyspepsia
There are two main types of functional dyspepsia – Postprandial Distress Syndrome (PDS) and Epigastric Pain Syndrome (EPS).
- Postprandial Distress Syndrome: characterized by symptoms that usually develop after meals, which include early satiety (where you can’t eat a full meal) and postprandial fullness (a prolonged, uncomfortable feeling of fullness after eating).
- Epigastric Pain Syndrome: involves pain or burning in the epigastric area (located between the lower end of the chest bone and the navel) without any correlation to meals. The pain is intense enough to be disrupting and is often persistent.
Understanding the Impact on the Body
In healthy individuals, the stomach relaxes to accommodate food during eating. However, in individuals with functional dyspepsia, the stomach may not relax fully resulting in discomfort, especially after meals. Some patients may also experience slower than normal emptying of the stomach contents into the small intestine. This delay can also lead to meal-related symptoms. Pain signals generated in the digestive tract may also be amplified in the brain of those affected by functional dyspepsia.
Understanding the Prevalence of Functional Dyspepsia
Functional dyspepsia, a frequent digestive disorder, affects around 10-15% of the global population. Despite its prevalence, many individuals do not seek medical help, leading to an underestimation of its exact spread. This condition doesn’t discriminate by age, affecting children and adults alike, although women seem to be marginally more susceptible than men.
While functional dyspepsia isn’t life-threatening, its chronic and persistent nature can profoundly disrupt an individual’s life. Consequences include absenteeism from work, disruptions in social activities, and an increased need for healthcare services. An individual living with functional dyspepsia often endures a frustrating, long-term battle with uncomfortable symptoms.
Symptoms and Causes of Functional Dyspepsia
Recognizing the Symptoms of Functional Dyspepsia
Functional Dyspepsia, also known as lingering stomach discomfort, manifests with symptoms similar to many other digestive disorders. Therefore, identifying the specific indications of Functional Dyspepsia is of utmost importance for healthcare providers and patients to secure an accurate diagnosis.
Typically, someone with functional dyspepsia feels discomfort or unease in the upper area of the stomach. Symptoms may include sensations of burning, bloating, nausea, premature fullness during meals, or excessive belching. The intensity of these experiences may fluctuate and isn’t necessarily tied to eating habits. Furthermore, these symptoms can vacillate, disappearing and reappearing over time. Alongside physical discomfort, the persistent nature of functional dyspepsia can lead to psychological disturbances like depression and anxiety due to the distressing impact on the individual’s quality of life.
Who is at Risk?
Despite being prevalent, Functional Dyspepsia does not discriminate by age or gender and can affect anyone at any stage of life. However, some studies have suggested that people with certain characteristics may be more likely to suffer from this condition. These include those who have a history of an infectious gastrointestinal disease, smoking, excessive consumption of alcohol, use of non-steroidal anti-inflammatory drugs (NSAIDs) or aspirin, and those under high emotional stress. It has been seen that women tend to report symptoms more often than men.
Exploring the Causes of Functional Dyspepsia
Functional Dyspepsia (FD) remains a bit of a mystery in the medical world as its exact cause is yet to be definitively pinpointed. This large unknown factor makes its diagnosis and treatment a bit more challenging. There are, however, several factors believed to have a role in the manifestation of this condition. Anomalies in gastric motility such as either a delay or hastening in the emptying of the stomach have been observed in FD patients. This abnormal activity in the muscle contractions of the stomach can be associated with FD symptoms.
One factor that could contribute to FD may include increased sensitivity to stomach acid or the stretching that occurs in the stomach following food intake. The amplification of these may be created by lifestyle choices like heavy smoking, excessive caffeine or alcohol intake. Psychological aspects including stress or anxiety have been observed to have links to FD, despite the intricate and currently incompletely understood nature of this relationship.
It’s also suggested that a bacterial pathogen, called Helicobacter pylori, may have a role in some FD cases, with ongoing studies exploring the precise connection. Notably, theories propose FD could be associated with abnormalities in brain-gut interaction, the vital system where the brain and gut communicate to regulate bodily functions. Disruption of the signals in this system may result in FD symptoms.
However, it’s important to note that our understanding of Functional Dyspepsia is still evolving and the specific causes can vary from person to person. Because of this, individuals identified as potentially having FD should be thoroughly evaluated by healthcare practitioners to ensure an accurate diagnosis and appropriate treatment plan.

Diagnosing Functional Dyspepsia
Getting to Know Functional Dyspepsia
Named one of the prevalent disorders related to the gastrointestinal tract, Functional Dyspepsia (FD) is known for triggering discomfort in the top section of the digestive tract. What defines FD is the sensation of being uncomfortably full during or just after meals, coupled with a painful or burning sensation felt in the epigastrium — the upper region of the abdomen. Uniquely, these symptoms often emerge in patients without an obvious cause, such as a stomach ulcer or any form of infection.
Medical Consultation
When a patient presents these symptoms, the doctor usually initiates a series of steps to diagnose if it is Functional Dyspepsia. The medical professional will ask about the patient’s medical history and perform a physical examination. The doctor will also ask about the specific location and nature of the pain, eating habits, lifestyle, and overall wellbeing. This helps differentiate Functional Dyspepsia from other gastrointestinal disorders like peptic ulcer disease or gastroesophageal reflux disease, and systemic diseases such as diabetes.
Diagnostic Tests and Procedures
Initially, blood tests may be carried out to screen for any underlying conditions such as anemia or infections. If the blood tests do not identify any anomalies, the doctor may proceed with additional diagnostic tests. An endoscopy is one such test in which a flexible tube with a camera is inserted through the mouth to observe the upper digestive system for any signs of ulcers or inflammation. Another test is a breath test which is used to check for Helicobacter pylori bacteria, a common source of stomach ulcers. Doctors may also recommend imaging tests such as ultrasound or computed tomography (CT) scan to rule out other causes of the discomfort.
Functional Dyspepsia vs Other Gastrointestinal Disorders
Diagnosing FD can be difficult because its symptoms are very similar to those of other gastrointestinal disorders. For instance, peptic ulcers and gastroesophageal reflux disease (GERD) also cause discomfort in the upper abdomen. However, these conditions usually have a clear identifiable cause, such as the presence of H. pylori bacteria or long term use of non-steroidal anti-inflammatory drugs in case of peptic ulcers, or weakening of the esophageal sphincter in case of GERD. The distinguishing factor of FD is that it is a functional disorder – this means that despite the ongoing symptoms, no organic cause is detected through tests.
ROME IV Criteria for Functional Dyspepsia
In the absence of a clear organic cause, the diagnostic criteria for FD rely largely on the symptoms reported by the patients. According to the ROME IV criteria (revised international standards for diagnosing FD), patients should have persistent or recurrent symptoms of epigastric pain or burning, postprandial fullness, or early satiety for at least three months with symptom onset at least six months prior to diagnosis.
Doctors often conduct a comprehensive consultation alongside standard diagnostic tests and procedures in order to correctly identify Functional Dyspepsia (FD). This allows them to differentiate it from other similar gastrointestinal conditions. The primary objective for medical professionals is to devise a treatment plan that can proficiently manage the symptoms and thereby, enhance the quality of life for individuals living with functional dyspepsia.

Treatment and Management Options for Functional Dyspepsia
Exploring Treatment Approaches for Functional Dyspepsia
A range of treatment options exist for functional dyspepsia. These often combine lifestyle modifications with medication strategies. The initial course of action typically involves dietary changes, whereby patients are advised to consume smaller, more frequent meals instead of three large ones, and to curtail the intake of fatty foods, caffeine, alcohol, and tobacco. Another recommendation is to avoid late-night meals and adhere to a regular eating schedule.
Beyond dietary measures, engaging in regular physical activity can prove beneficial in controlling the symptoms of functional dyspepsia. Regular exercises foster a properly functioning digestive system and help to mitigate stress. Research indicates that carrying out moderate-intensity exercise for roughly 30 minutes a day can potentially enhance digestion and lessen symptoms associated with dyspepsia.
Finally, mind/body interventions can significantly contribute to managing functional dyspepsia. Techniques such as cognitive-behavioral therapy, hypnotherapy, meditation, and biofeedback may help to alleviate symptoms by moderating stress levels and invoking relaxation.
Medication Therapies for Functional Dyspepsia
Medications can also play a role in managing functional dyspepsia. Antacids and acid blockers like H2 blockers and proton pump inhibitors can reduce stomach acid and alleviate symptoms. Prokinetic agents might be prescribed to strengthen the muscles in the gastrointestinal tract and speed up the emptying of the stomach. Additionally, antidepressants in low doses are used to alleviate abdominal pain associated with functional dyspepsia.
Long-term Management Strategies
As for long-term strategies for managing functional dyspepsia, establishing a regular eating and exercise schedule, managing stress, and sticking with medications prescribed by the healthcare provider are crucial. In addition to regular medical visits, patients should learn to identify and avoid specific trigger foods or activities that worsen their symptoms.
Cognitive-behavioral therapy and other psychological therapies help to teach the patient coping strategies to manage the condition and improve the quality of life. These strategies focus on altering thought patterns and behaviors that may be contributing to the symptoms of functional dyspepsia.
Minimizing Impact on Daily Life
Living with functional dyspepsia can significantly impact a person’s daily life, therefore learning effective ways to minimize these impacts is essential. The strategies mentioned earlier like regular physical activity, dietary changes, and stress management can help reduce symptoms and improve daily functionality. Patients should be encouraged to lead a normal life as much as possible, focusing on tasks and events aside from their symptoms.
Furthermore, seeking support from family, friends, or other people with functional dyspepsia can provide psychological comfort and practical advice on dealing with this chronic condition.

Armed with an understanding of functional dyspepsia, readers can better comprehend how this condition may influence their own lives or those of loved ones. Recognizing the symptoms and causes can prompt timely medical consultations and the initiation of appropriate diagnostic processes. Even more importantly, being aware of the diverse treatment options and long-term management strategies increases the likelihood of effectively controlling functional dyspepsia. Ultimately, this comprehensive knowledge serves not only to elevate public consciousness on this prevalent gastrointestinal disorder but also to empower individuals towards informed health decisions and enhanced quality of life.