Interstitial Cystitis is a chronic bladder issue that significantly affects the quality of life of those suffering from it. Characterized by persistent bladder pain, frequent urination, and a sense of urgency to urinate, the condition requires effective management and treatment. One such treatment gaining traction is bladder stretching, a procedure aimed at increasing bladder capacity whilst reducing urination frequency. This article delves into understanding Interstitial Cystitis, the methodology of bladder stretching, its effectiveness, risks, and real-life case studies. In addition, it explores alternative treatments so that readers can take an informed decision about their health conditions.
Understanding Interstitial Cystitis
Understanding Interstitial Cystitis
Interstitial Cystitis, also known as painful bladder syndrome, is a chronic condition that leads to bladder pain and pressure. This condition is often accompanied by persistent and urgent urination. The condition itself is enigmatic as it differs greatly among individuals. While some may experience mild discomfort, frequency, or urgency, others grapple with severe pain. The walls of the bladder are lined with multiple layers of tissue that serve as a barrier to toxins in urine. However, with Interstitial Cystitis, these layers are often disrupted, enabling toxins to irritate the bladder wall.
Causes, Symptoms, and Effects on The Body
The exact cause of Interstitial Cystitis is unknown. However, several theories suggest potential triggers like an autoimmune response, heredity, infection, or allergy. The key manifestations of the condition involve frequent urination, urgent need to urinate, pain in the bladder, and discomfort in the pelvic region. As the bladder fills, the pain might increase, and relieved temporarily by urination.
The impacts of interstitial cystitis on the body extend beyond the bladder. Research shows that this condition adversely influences mental health, quality of life, and sleep. In many cases, patients with interstitial cystitis also report of other health problems such as irritable bowel syndrome, fibromyalgia, and chronic fatigue syndrome.
Bladder Distention: A Treatment Option for Interstitial Cystitis
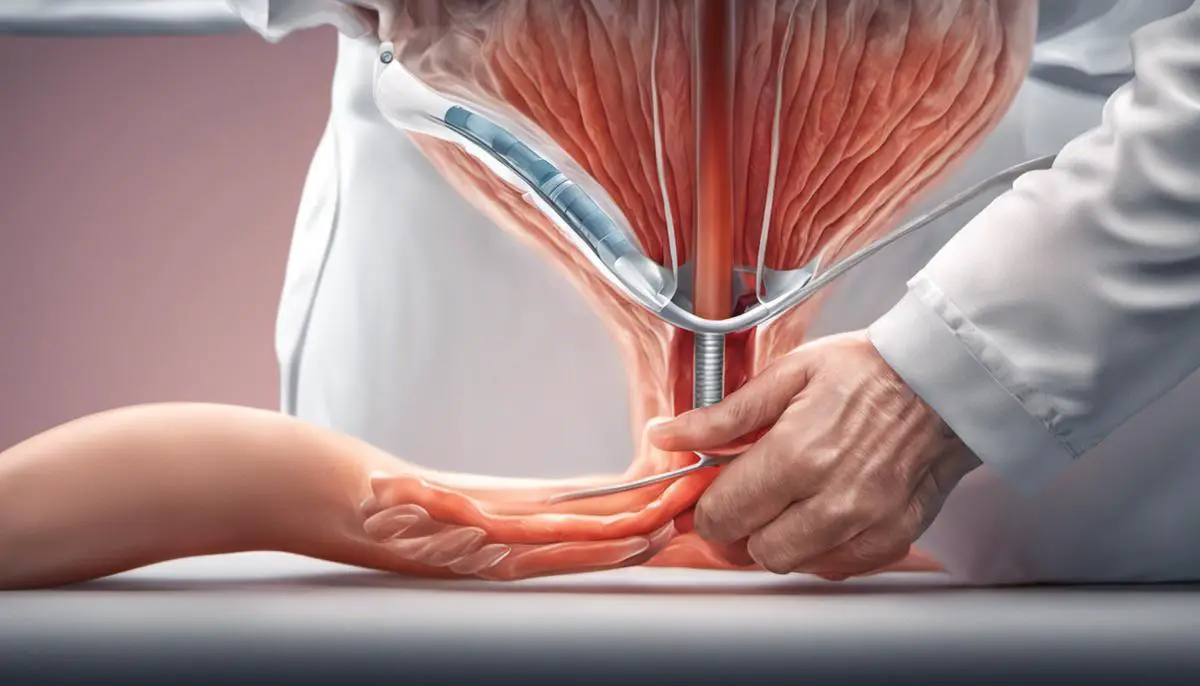
Bladder distention, most commonly referred to as bladder stretching, is a potential treatment method for Interstitial Cystitis. This procedure comprises the inflation of the bladder with a fluid or gas, causing it to stretch. It’s believed that this stretching can amplify bladder capacity and disrupt pain signals being sent from the bladder to the brain, thereby lessening symptoms.
To undertakes this bladder distention treatment, doctors generally utilize cystoscopy, a diagnostic method that gives them a visual of the inside of your bladder. After undergoing bladder stretching, for some patients, there may be a temporary alleviation of symptoms, such as reduced frequency of urination and decreased pain. However, this relief isn’t a long-term solution, and symptoms may resurface over time.
It’s crucial to understand that bladder stretching isn’t a full-fledged cure for Interstitial Cystitis. It’s merely a symptomatic treatment, typically suggested to those who haven’t seen much improvement with other treatments. There could be side effects, including bladder rupture (though this is a rare case) and a temporary increase in pain or urinary frequency post-procedure. It’s therefore incredibly important to have a thorough discussion about the procedure’s potential pros and cons with your medical provider.
With the advancement of medical research, potential exploration of other treatment options like medications, nerve stimulation, and lifestyle changes (like diet modification) are presently on the rise. However, bladder stretching continues to be a key tool for many suffering from Interstitial Cystitis to manage their condition.

Photo by towfiqu999999 on Unsplash
Bladder Stretching – What it Implies
Understanding Interstitial Cystitis and the Role of Bladder Stretching
Interstitial Cystitis (IC), also recognized as Painful Bladder Syndrome, is a chronic condition triggering discomfort, pressure, and pain in the bladder and pelvis. Bladder stretching, medically known as hydrodistention, can be a potential treatment option for those with IC.
The procedure focuses on stretching the bladder to its maximum capacity under anesthesia with the objective to decrease urinary urgency and frequency. This is achieved by inserting a cystoscope (a thin tube equipped with a light and camera) into the urethra and infusing a sterile water or saline solution to aid the stretching process.
Procedure and Safety of Bladder Stretching
Bladder stretching or hydrodistention is an outpatient procedure, usually performed under general anesthesia, lasting between 15 to 30 minutes. It can be part of a diagnostic procedure to identify the features of IC such as Hunner’s ulcers, a specific type of lesion in the bladder lining.
The safety of the procedure is generally high, but as with any invasive procedure, there can be side effects and risks. Some patients may experience increased bladder pain and urinary frequency for a few days following the procedure, but these symptoms often subside with time. Other, rare, risks include bladder rupture or perforation, urinary tract infection, and hematuria – the presence of blood in the urine.
Most patients report a decrease in pain and urinary urgency after the procedure. However, the relief can be temporary, and the duration of symptom relief can vary from patient to patient.
Understanding the Role of Bladder Stretching in IC Treatment
Bladder stretching, often combined with other treatments like medication, bladder instillations, or nerve stimulation, plays a critical role in the multifaceted approach to treating Interstitial Cystitis (IC). This procedure is generally recommended for individuals with moderate to severe IC symptoms who are unresponsive to conventional management strategies.
The primary goal of bladder stretching is to enhance the functional capacity of the bladder and numb the nerves within the bladder wall. This, in turn, leads to a reduction in pain and a decrease in the frequency of urination. Still, the precise mechanism by which bladder stretching alleviates pain and other IC symptoms remains a mystery.
In summary, bladder stretching, also known as hydrodistention, is a regular element in the treatment plan for patients with Interstitial Cystitis. Nevertheless, it’s crucial to recognize the potential risks associated with the procedure and to discuss these with your healthcare provider before commencing treatment. Remember, while bladder stretching is valuable in IC treatment, it’s only one component of a comprehensive IC management strategy, and when combined with other approaches, it may yield optimal results.

Effectiveness and Risks of Bladder Stretching
A Closer Look at Interstitial Cystitis and Bladder Stretching
Interstitial Cystitis (IC), also referred to as painful bladder syndrome, is a persistent bladder health condition typified by pelvic pain and pressure in the bladder. Bladder stretching, or bladder distention or hydrodistention as it is commonly known, is one of the techniques utilized to manage IC symptoms. This procedure involves the inflation of the bladder with fluid or gas, thereby stretching the bladder walls. This is believed to ease IC symptoms by boosting bladder capacity or interfering with the nerves that transmit pain signals from the bladder.
Effectiveness of Bladder Stretching for Treating Interstitial Cystitis
While bladder stretching has been used for years to diagnose and treat Interstitial Cystitis, there remain questions about its effectiveness. Some patients have reported a reduction in their symptoms following this procedure. In a 2007 Urology journal study, conducted on a population sample of 55 IC patients, more than half of the participants reported significant relief for 3 months after a single procedure.
However, longer-term relief is inconsistent. For example, in another study published in the “Journal of Urology,” only 25% of those treated with bladder distention showed symptom improvement after five years. This affirms the need for repeated bladder distention procedures in certain cases.
Limitations and Risks
Bladder stretching is not without risks. Complications can include bladder rupture, infection, or urinary retention. Other side effects can include more frequent urination, persistent discomfort or pain, and in rare cases, bladder wall tears. Additionally, bladder distention does not effectively treat all IC symptoms – while it may help with pain, studies indicate it often doesn’t significantly reduce urgency or frequency.
Considerations of Bladder Stretching as a Treatment Option
As with any medical procedure, it’s crucial to discuss the potential benefits and risks with a healthcare provider before deciding on bladder distention as a treatment option. Your provider can help you assess your individual circumstances, including your symptoms, overall health status, and personal preferences, in making a decision. Other treatment options, such as medication, physiotherapy, or nerve stimulation, may be alternatives if bladder distention isn’t the optimal choice.
Research Findings: A Balanced View
The weighted benefits and risks indicate that bladder distention can potentially help manage IC symptoms, but it’s not an ideal solution for all patients. Several medical research data support this balanced view, indicating that while bladder stretching can provide short-term relief in some cases, long-term effectiveness is inconsistent and the procedure comes with a considerable potential for side effects. Further, while bladder stretching may be part of a multimodal treatment plan, it’s not usually considered as the first-line treatment for IC.
Exploring the Scope of Research
There exists a significant divergence in how patients respond to bladder distention, underlining the importance of continued intensive research to delineate possible beneficiaries of this treatment modality. Multiple ongoing studies are currently trying to refine the process by targeting the bladder’s pain signaling pathways. Alongside, explorations into other cutting-edge treatment avenues for Interstitial Cystitis (IC) are also underway. The continuous evolution of scientific comprehension of IC will undoubtedly enhance the spectrum of available effective treatment options.
Case Studies for Bladder Stretching Treatment
Patient Scenario: Young Athletic Female
Let us consider the case of a 25-year-old professional athlete who has battled the symptoms of Interstitial Cystitis (IC) since her formative teenage years. Given her physically exhaustive routine, the recurrent physical discomfort stemming from IC symptoms like painful urination and chronic pelvic pain significantly dented her performance. Her condition remained largely unchanged despite numerous trials with traditional therapies, prompting her to seek a bladder stretching treatment, also known as hydrodistention.
The outpatient procedure involved general anesthesia, where her bladder was filled with a sterile saline solution, causing it to stretch. The primary goal was to temper the IC symptoms by thwarting pain signals transmission.
Post-treatment, the athlete experienced a sudden abatement in urination frequency and pain intensity. She was able to get back to her maximum training regime six months after the procedure. This case underscores the potential of bladder stretching treatments in significantly bolstering a patient’s quality of life.
Patient 2: Retired Male with Long History of IC Symptoms
Another case study focuses on a 65-year-old retired male who had been suffering from the symptoms of IC for over 20 years. Despite being medically managed with medications and lifestyle modifications, his quality of life was considerably diminished, particularly his sleep quality due to frequent nighttime urination.
He decided to undergo bladder stretching treatment as an alternative approach. After the procedure, the patient experienced a significant decline in his symptoms. Nighttime urination frequency was reduced, and overall pain levels were dramatically decreased, allowing him to enjoy a more restful sleep.
One year post-procedure, the patient’s symptoms showed no signs of relapse. The results of this treatment played a substantial role in his overall health improvement and quality of life, emphasizing the benefits bladder stretching treatments can have for sufferers of IC.
Patient 3: Middle-aged Professional Female
The third case involves a 40-year-old professional woman who had been dealing with IC symptoms for five years. Despite trying various oral medications and physical therapy, she continued to experience chronic pelvic pain and urinary urgency.
The woman opted for bladder stretching treatment as a last resort. After the procedure, she experienced a gradual decrease in pelvic pain and urinary urgency over a period of weeks. Six months after the procedure, she reported a significant improvement in her IC symptoms, allowing her to regain control over her daily life and work productivity.
While exploring treatments for Interstitial Cystitis, bladder stretching has shown promising potential, especially when conventional therapies fail to provide desired relief. However, it’s important to note that each patient’s case is unique, making the results of treatments vary widely. It’s therefore crucial for each patient to have a thorough conversation with their healthcare provider to determine the most suitable plan of action.

Alternative Treatments for Interstitial Cystitis
Pharmaceutical Approaches: Improving Bladder Health with Medication
Another common treatment approach for Interstitial Cystitis (IC), commonly referred to as ‘painful bladder syndrome’, revolves around pharmaceutical interventions. These include orally consumed medications, drugs directly instilled into the bladder – known as intravesical drugs, and injections. Most commonly, pain relievers, antihistamines, and tricyclic antidepressants are prescribed to manage the discomfort associated with IC. A specific FDA-approved drug for IC, Elmiron, works by coating the bladder walls, thereby protecting it from aggravating substances present in urine.
Bladder Stretching: A Potential Respite from IC Pain
Hydrodistention or bladder stretching, is a procedure where the bladder is filled with water or gas, stretching its walls. This treatment is often employed for patients with IC, as it can reduce symptoms for a few weeks or months. The procedure works under the hypothesis that stretching the bladder can help increase its capacity and reduce the frequency of painful contractions. However, the benefits are often temporary and repeated procedures may be required. Some patients may experience more severe symptoms after the procedure, so it’s essential to discuss the potential risks and benefits with your healthcare provider.
Physical Therapy: A Non-Invasive Approach to Manage IC
Physical therapy, particularly pelvic floor exercises, can help manage the pain and other symptoms of IC. Since interstitial cystitis can cause pelvic muscles to tighten in response to bladder pain, targeted therapy can help relax these muscles and promote better bladder functionality. Patients can consult with a physical therapist who specializes in pelvic floor disorders to get a tailored exercise plan.
Nutritional Regime: Dietary Modifications to Alleviate IC Symptoms
Research has revealed a connection between diet and IC symptoms. Certain foods and drinks can aggravate the disorder. These often include caffeinated beverages, alcohol, foods high in sugar, and spicy or acidic foods. To determine a diet best suited to manage individual cases of IC, some people may undertake an elimination diet, systematically removing and reintroducing different foods into their diet to identify potential triggers.
Alternative Therapies: Thinking Outside the Medicine Box
Apart from conventional treatments, some patients turn to alternative therapies for managing their IC symptoms. Acupuncture, for instance, has been reported to help some patients by relieving pain and pressure in the pelvic region. Bladder training (retraining your bladder to hold urine for increasing periods) and nerve stimulation treatments may also prove beneficial for some people.
Support and Counseling: Managing the Emotional Toll of IC
Living and managing a chronic disorder like IC can take a significant emotional toll on a person. It can cause anxiety, depression, and stress in patients. Therefore, counseling or psychological therapy should also be considered as part of a holistic approach towards managing IC. Support groups can also be of immense help to people suffering from IC by providing a platform for shared experiences and coping strategies.
As IC is a multifaceted condition, a combination of treatments may be necessary for optimal symptom management. It’s crucial for patients to consult their healthcare providers in order to devise a treatment plan that effectively targets their individual symptoms.

Photo by laurynasm on Unsplash
Interstitial Cystitis is an ongoing struggle for many, however, treatments like bladder stretching seem to offer a glimmer of hope. While this treatment has proven efficacy for many, it’s important to remember that each person’s experience with Interstitial Cystitis is unique – what might work for one might not work for another. The exploration of different therapies, including lifestyle changes, physical therapy and medication, is critical for individual health management. Ultimately, being informed and understanding one’s own body, along with a proactive discussions with healthcare providers, may lead to the most effective treatment strategies for those living with Interstitial Cystitis.
