Interstitial Cystitis (IC), often known as painful bladder syndrome, is a chronic condition impacting a multitude of individuals worldwide, bringing about significant physical discomfort and emotional distress. This intricate health issue is defined by recurring pain or pressure in the bladder and pelvic region, along with an urgent and frequent urge to urinate. This complex condition not only challenges the physical wellbeing but also profoundly impacts the mental health of individuals, thus necessitating holistic understanding and comprehensive approach for effective management. Our exploration of IC starts with defining the disease, followed by insights into its symptoms, causes, and diagnosis methods. We then delve into the spectrum of treatments available, explaining the nuances of medications, physical therapies, and potential surgeries. The subsequent section tackles lifestyle modifications, offering practical steps to manage IC’s discomforts and enhance one’s quality of life. Finally, we address the psychological aspects of living with IC and the importance of a robust support network, ushering a balanced view of managing IC.
Understanding Interstitial Cystitis
Understanding Interstitial Cystitis
Interstitial Cystitis (IC) is a chronic condition that causes discomfort, pain, or pressure in the bladder area, and predominantly affects women. Also known as painful bladder syndrome, IC can range from mild to severe symptoms which may interfere with one’s quality of life. The exact cause of IC is unclear, although certain factors like defects in the bladder lining, an autoimmune reaction, an infection, heredity, and allergies can contribute to its development.
The symptoms of IC are varied and can change over time, with periods of flare-ups alternating with remissions. Common symptoms often include chronic pelvic pain, a persistent and urgent need to urinate, frequent urination, discomfort or pain during sexual intercourse, and in some cases, pain in the lower back, thighs, or other parts of the body.
Diagnosis of Interstitial Cystitis
Diagnosing IC can be tricky as the symptoms often mimic other urinary-related disorders. To identify IC, healthcare practitioners might use processes like a urine analysis to rule out urinary tract infections, a bladder diary to log the frequency of urination, and the level of pain, a cystoscopy to inspect the bladder lining, or a biopsy for ruling out bladder cancer, and also to check for any bladder abnormalities.
Managing Interstitial Cystitis Pain
Managing IC pain requires a combination of lifestyle changes, medication, physical therapy, and at times, surgery. Due to the varying nature of IC, what works best for one patient might not work for another. Hence, a tailored approach is essential.
Certain dietary changes, such as the elimination of bladder irritants like caffeine, citrus fruits, spicy foods, and alcohol, can help in reducing the symptoms. Hydration is crucial, but overhydration can aggravate the bladder. Consequently, striking a balance and hydrating adequately without overdoing it is essential.
Physical therapy can aid in relaxing muscle tension in the pelvic area and reducing pain. Techniques like biofeedback, heat and cold therapy, pelvic floor exercises, nerve stimulation, bladder training, and physical exercises can be beneficial.
Medications can also significantly aid in IC management. Oral medicines, bladder instillations, non-steroidal anti-inflammatory drugs (NSAIDs), antihistamines, and nerve pain medications can help in improving symptoms over time. In severe and unresponsive cases, surgical intervention might be a viable route.
Self-care practices, like stress management, can play a vital part in managing IC pain. Chronic illness can cause emotional distress, which in turn can exacerbate physical symptoms. Hence, incorporating tools like gentle exercise, meditation, relaxation techniques, and getting enough rest can enhance the overall well-being and quality of life. Also, support from a therapist, counselor, or a support group can provide much-needed emotional comfort.
Understanding the Complexity of Managing Interstitial Cystitis Pain
Interstitial Cystitis (IC) presents a complex challenge in the medical world due to its elusive nature, an ambiguity of causes, a wide range of symptoms, and the absence of a universal treatment. This complexity often results in delayed diagnosis, the necessity of trial-and-error with treatments, and the potential for significant frustration for patients. Additionally, the chronic pain and consistent disruption of daily routines due to frequent bathroom trips can lead to considerable emotional stress. As such, it’s imperative to prioritize raising awareness about IC, expedite early diagnosis, and promote the importance of holistic patient care.

Treatments for Interstitial Cystitis
Exploring Medication Options for Interstitial Cystitis (IC)
While a definitive cure for IC remains elusive, a variety of medications are available to help manage the symptoms and reduce discomfort. These can range from oral drugs to treatments directly instilled into the bladder. Commonly prescribed medications for IC include pain relievers, antidepressants, and antihistamines. For some, a drug known as pentosan polysulfate sodium (Elmiron) may provide relief by aiding in the repair of the bladder wall.
However, all medications come with potential side effects that need to be taken into account. For instance, pentosan polysulfate sodium might lead to headaches and diarrhea, while anti-depressants can cause symptoms like a dry mouth or constipation. Hence, consistent medical supervision is essential when using these medications long-term to ensure effective management of potential side effects.
Physical Therapies
Physical therapy often plays an essential part in managing IC pain, particularly pelvic floor physical therapy. Tightening, spasms or tension in the pelvic floor muscles, can contribute to IC-related discomfort. A qualified physical therapist can provide exercises to help relax these muscles and subsequently relieve pain.
Physical therapies may also involve neurostimulation techniques, such as transcutaneous electrical nerve stimulation (TENS), which can help alleviate IC-related pain by increasing blood flow to the bladder and strengthening pelvic muscles. However, outcomes can vary, and these therapies may not work for every patient.
Surgeries for Interstitial Cystitis
When other treatments fail to manage IC symptoms, surgery is considered as a last resort. Some surgical procedures aim to increase the size of the bladder using segments of the patient’s intestine, also known as bladder augmentation. Other surgeries may involve installing an artificial urinary sphincter or managing the nerves affecting bladder sensations.
Surgical treatments for IC can bring about significant changes to a person’s daily life, and all have potential risks and side effects. Bladder augmentation, for example, may require patients to empty their bladder using a catheter permanently. Furthermore, like all invasive procedures, there is always a risk of infection and complications due to anesthesia.
Living with Interstitial Cystitis: Quality of Life and Pain Management
For those living with Interstitial Cystitis (IC), the path to improved quality of life often lies in effective pain management. This isn’t just about finding the right medical treatments – it also involves making considered lifestyle modifications. Altering your diet, learning stress management techniques, and swapping to loose clothing can all help to reduce the frequency and intensity of the painful flares common to IC.
It’s important to recognize that while IC can be a chronic, life-disrupting condition, a range of options for symptom and pain management are available. Effective management starts with a strong patient-doctor relationship. Working closely with your healthcare provider to develop a personalized treatment plan can help balance the need for symptom control, the management of potential side effects, and the overarching goal of quality of life preservation.

Photo by towfiqu999999 on Unsplash
Lifestyle Modifications for Interstitial Cystitis
Dietary Changes: A Key Tool in Interstitial Cystitis Management
One powerful tool in the fight against Interstitial Cystitis is diet. Certain foods and drinks can make IC symptoms worse – caffeine, alcohol, spicy foods, citrus fruits, and artificial sweeteners are often the main culprits. Conversely, those with IC may find that a diet emphasizing calcium and rich in vitamin D can greatly alleviate symptoms. But navigating these dietary changes can be tough, so it’s highly recommended to engage the services of a dietitian. These professionals can help you identify personal triggers, and can also provide balanced meal plans that consider your nutritional needs.
Remember, everyone’s different – what worsens symptoms for one person may not do the same for another. To help identify your triggers, it can be incredibly useful to maintain a food diary.
Urinating Habits and Fluid Intake
Overstrain during urination can exacerbate IC pain. To alleviate the strain, it is recommended to urinate regularly, ideally every three to four hours. Additionally, drinking an adequate quantity of water throughout the day — six to eight cups — can help dilute urine, reducing irritation to the bladder lining. However, it is best to avoid gulping large amounts of fluid at once, as this could overwhelm the bladder and increase urgency or frequency.
Practicing Bladder Training Techniques
Bladder training can be a necessary home management technique for IC pain. The goal of bladder training is to gradually extend the time between trips to the bathroom. This training helps restore the bladder’s normal function and reduce symptoms of frequency and urgency. A common technique is the use of peaceful distractions whenever there arise an urge to urinate. Consulting a Continence Advisor or a Physiotherapist would be beneficial when approaching bladder training.
Exercises for Interstitial Cystitis
Certain exercises can be helpful in managing IC pain. Regular physical activity like low-impact cardio, especially walking, can reduce IC pain by reducing inflammation and enhancing overall health. Similarly, pelvic floor exercises under the guidance of a physical therapist might help strengthen the supporting muscles of the pelvic organs and potentially reduce bladder pressure.
Stress Management and Interstitial Cystitis
Stress has been observed to worsen IC symptoms in many patients. Incorporating stress management techniques, like relaxation exercises, mindfulness, yoga, and deep-breathing exercises, can aid in reducing IC related pain and discomfort. Cognitive-behavioral therapy is another effective approach to manage stress and the mental toll that chronic pain can take.
Wear Comfortable Clothing
Tight, form-fitting clothing can increase discomfort for those with IC, especially pants that put pressure on the abdomen. Opting for looser, more comfortable clothes, can be one more step toward managing daily IC symptoms.
Use of Heat Therapy
Applying a heating pad to the lower abdomen can help relieve IC pain by relaxing pelvic muscles and reducing bladder pressure. However, the heated pad should be used on a low setting to avoid skin burns.
As an important starting point, it’s fundamental to keep in mind that every individual’s experience is unique and approaches that are effective for one person may not apply to another. Therefore, the role of a healthcare professional becomes paramount in guiding each individual through personalized lifestyle alterations aimed at managing Interstitial Cystitis pain.

Psychological Impact and Support for IC Patients
Understanding the Psychological Ramifications of Interstitial Cystitis (IC)
Experiencing the persistent discomfort of Interstitial Cystitis (IC), a chronic pain disorder, goes beyond physical affliction. It can also impose substantial psychological burden due to constant pain, unpredictable exacerbations, and the often elusive search for effective solace. This can manifest as elevated levels of stress, anxiety, depression, and diminished quality of life. The feelings of overwhelming physical pain, fear of escalating symptoms, and frustrations concerning the disease often cloud patients’ minds. These factors can spawn a perpetual cycle where chronic pain triggers chronic stress, possibly potentiating both the physical and psychological symptoms.
Importance of Psychological Support for IC Patients
Given the intertwined nature of physical pain and mental health, psychological support becomes crucial in managing IC pain. A multi-disciplinary treatment approach involving clinicians, psychiatrists, and psychologists can help patients better manage their condition. Cognitive-behavioral therapy (CBT) is one intervention that has shown promise for IC patients. CBT can help patients learn effective coping mechanisms, reduce pain perception, relax the bladder, and combat negative thoughts.
Depression, Anxiety, and IC
A significant proportion of IC patients experience depression and/or anxiety, which can further intensify their physical symptoms. Research shows that the risk of depressive and anxiety disorders is higher among IC patients than the general population. Consequently, it becomes necessary for those struggling with these issues to seek professional help. Antidepressant and antianxiety medications can potentially alleviate some IC-related pain while addressing mental health symptoms.
Role of Patient Communities and Support Groups
In dealing with IC, patient communities and supportive social networks can be valuable resources. Participating in support groups, either in person or online, can provide a venue to share experiences, learn from others’ coping strategies, and foster feelings of acceptance and understanding. Support from peers can also reduce feelings of isolation which can be a common experience for individuals with chronic pain conditions.
Professional Psychological Help for IC
Mental health professionals can provide tailored coping strategies to deal with the stressors associated with chronic pain conditions like IC. These strategies may include relaxation techniques, biofeedback, pain education, and cognitive restructuring. Psychotherapy can assist in reducing discomfort and urinary urgency by teaching the person to gain control over their bladder, rather than feeling controlled by it. Additionally, therapists can help improve quality of life by addressing related mental health issues such as depression and anxiety.
To conclude, managing the psychological impact of IC involves a holistic treatment approach that includes medical management of the condition, psychological interventions, and community support. Recognizing and addressing the psychological effects of IC can significantly enhance the overall treatment effectiveness, enhance the patient’s quality of life, and reduce the likelihood of pain exacerbation.
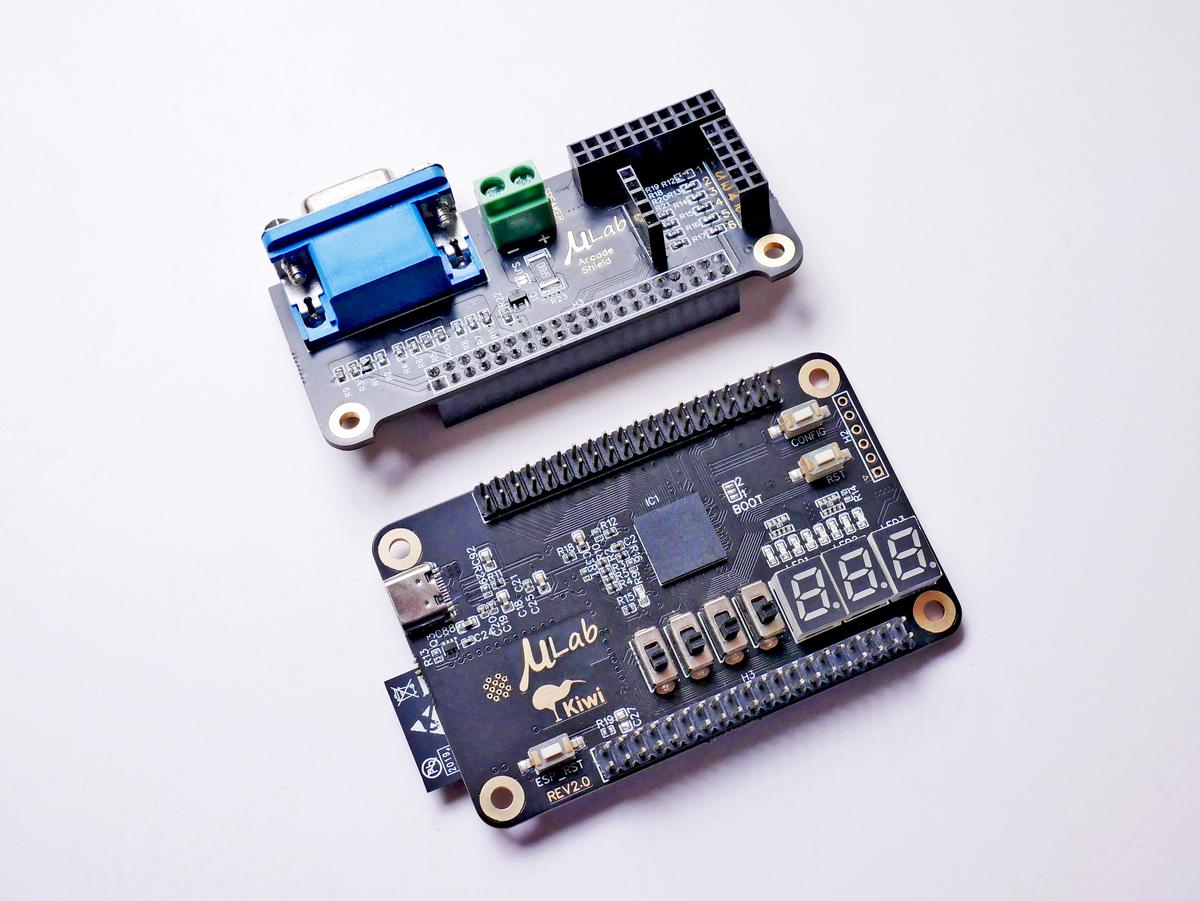
Photo by vishnumaiea on Unsplash
Navigating the turmoil of life with Interstitial Cystitis (IC) is a demanding journey, filled with frequent therapies, lifestyle adjustments, and emotional ups and downs. However, equipped with comprehensive understanding and appropriate resources, one can effectively manage the physical discomfort and alleviate the psychological distress associated with IC. Implementing suitable treatment modalities combined with the necessary lifestyle changes can significantly improve the quality of life for IC patients. Besides medical interventions, fostering resilience and seeking psychological support are fundamental for an all-encompassing approach to managing IC. Patient communities and support groups can offer immense strength and reassurance, reinforcing the conviction that IC patients are not alone in this journey. Remember, in the face of chronic conditions like IC, knowledge is power, self-care is vital, and strong support networks are indispensable.
